Understanding Neuropathy
Neuropathy describes conditions that arise when nerves in the body are damaged or malfunction, leading to pain, tingling, numbness, and muscle weakness. This nerve impairment can result from diabetes, autoimmune diseases, infections, traumatic injuries, or exposure to harmful substances. Understanding the underlying cause is critical for successful management.
Early identification and a proactive approach to care are essential, as neuropathy can be progressive if left untreated. Fortunately, effective options for neuropathy treatment Jacksonville, FL are available, and tailored interventions can greatly improve quality of life and symptom control. These treatment plans often include a combination of lifestyle changes, physical therapy, medications, and targeted therapies to address symptoms and their root causes.
Common Types of Neuropathy
Peripheral Neuropathy
Peripheral neuropathy is the most prevalent form of the condition, impacting the nerves that bridge communication between the brain, spinal cord, and the rest of the body. Typical symptoms include numbness, tingling, burning sensations, and sharp pain in the hands and feet. Causes are varied, with diabetes being the leading risk factor, but it can also arise from nutritional deficiencies, certain medications, infections, and hereditary conditions.
Autonomic Neuropathy
Autonomic neuropathy targets the nerves that regulate automatic body functions such as blood pressure, digestion, bladder function, and heart rate. Its symptoms often include excessive or insufficient sweating, digestive disturbances like constipation or diarrhea, dizziness upon standing, and difficulty controlling bladder and bowel function. Chronic conditions such as diabetes, chronic alcoholism, or autoimmune disorders can trigger autonomic neuropathy.
Focal Neuropathy
This type of neuropathy involves damage isolated to a single nerve or a group of nerves, typically in the hand, head, torso, or legs. Carpal tunnel syndrome, where the median nerve is compressed at the wrist, is a classic example. Symptoms often develop suddenly and can cause intense pain, muscle weakness, or paralysis in the affected area. Focal neuropathy may also result from injury, repetitive motion, or nerve entrapment.
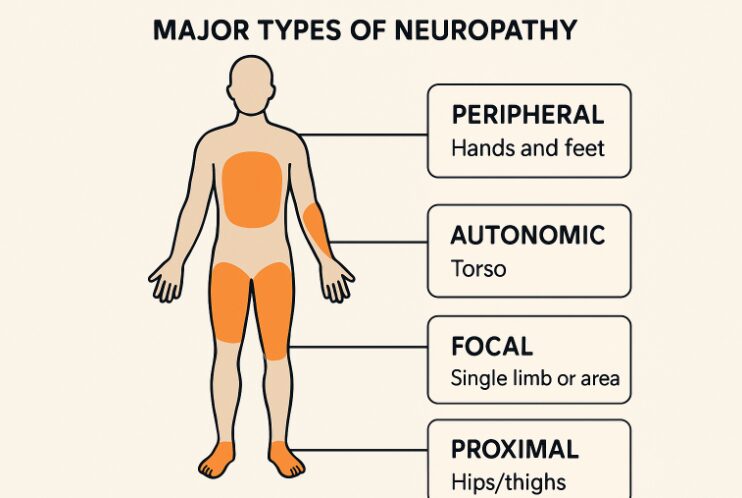
Proximal Neuropathy
Proximal neuropathy, also known as diabetic amyotrophy, primarily affects the hips, thighs, buttocks, or legs. It generally presents as sudden, severe pain followed by muscle weakness and difficulty moving the affected limb. This type is more common among older adults with type 2 diabetes and may have a slower recovery process compared to other nerve disorders.
Treatment Approaches for Neuropathy
Medications
- Pain Relievers: Over-the-counter options like acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) can help manage mild pain, while more severe pain might require prescription painkillers.
- Antidepressants: Tricyclic antidepressants such as amitriptyline and serotonin-norepinephrine reuptake inhibitors (SNRIs) like duloxetine are used for their pain-modulating effects.
- Anticonvulsants: Medications such as gabapentin and pregabalin, often used for epilepsy, can calm overactive nerves and reduce neuropathic discomfort.
Physical Therapy
Physical therapy plays an important role in the recovery and management of neuropathy, especially for those experiencing muscle weakness, loss of balance, or limited mobility. Targeted exercises and stretches can strengthen affected muscle groups, boost coordination, and reduce fall risk. Additionally, transcutaneous electrical nerve stimulation (TENS) has been shown to help some patients manage neuropathic pain more effectively.
Lifestyle Modifications
- Blood Sugar Control: Carefully managing blood glucose levels is paramount for individuals with diabetic neuropathy, as it helps halt the progression of nerve damage and can relieve symptoms over time.
- Healthy Diet: Proper nutrition is vital, particularly diets rich in B vitamins and antioxidants, which support nerve repair and health.
- Regular Exercise: Gentle physical activity like swimming, walking, or yoga promotes better circulation, fortifies muscles, and can help manage pain and fatigue associated with neuropathy.
Alternative Therapies
Several patients with chronic neuropathy symptoms turn to alternative or complementary therapies for symptom relief. Acupuncture, for example, stimulates nerve pathways and promotes natural pain suppression. Some use dietary supplements, such as alpha-lipoic acid and vitamin B12, for their antioxidant and neuroprotective properties, but medical supervision is recommended before starting any supplementation.
Recent Advancements in Neuropathy Treatment
Neuropathy research continuously reveals new ways to treat and potentially reverse nerve damage. Innovative techniques like stem cell therapy and gene therapy are being studied for their ability to promote nerve regeneration at a cellular level. Wearable technology is also emerging as a tool to assist with nerve stimulation, pain reduction, and real-time symptom tracking, promising greater autonomy for patients.
Researchers are optimistic that these advancements, in combination with traditional therapies, may enhance treatment outcomes dramatically over the coming years.
Living with Neuropathy
Successfully managing neuropathy involves a comprehensive, individualized care plan combining medical intervention, physical and lifestyle therapies, and ongoing support. Open communication with healthcare providers is crucial for monitoring symptoms, optimizing treatments, and promptly addressing new or changing issues. Patients should embrace healthy habits, stay informed about new treatment options, and draw on clinical expertise and community resources for optimal well-being.















































Leave a Reply